Digital companion on WhatsApp keeps patients safe outside the hospital
17 de dezembro de 2024By Roseli Andrion | FAPESP Innovative R&D – Going through a health treatment requires dedication and discipline, not to mention the fact that being diagnosed with a disease is stressful in itself. The ability to engage with this process requires commitment, which can often be a major challenge, especially since much of the information and procedures are completely new to the patient.
This is because they get a lot of information and have to monitor it themselves, i.e. decide what is important and what is not. If they feel there’s something unusual, they go to the hospital – but it may be something that could have been solved in a different way. Other times, they don’t go to the health unit when it’s important, and a complication that could have been caught early becomes serious and lands them in the ICU.
For some years now, it has been recognized that the best environment for a patient’s recovery is their own home. On the other hand, there is a risk that they won’t know if they are doing well – not least because they don’t have the intensive care offered in a hospital – and will feel the need to stay in the care unit.
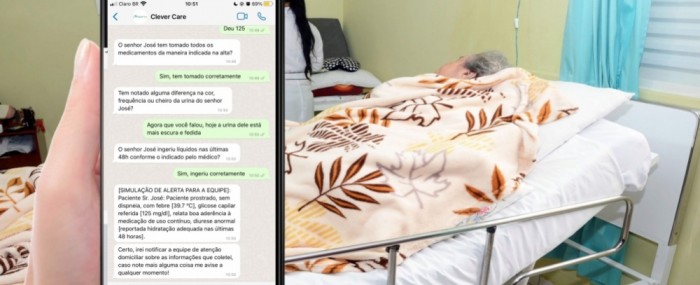
With so much technology in the hands of patients, one option is to use it to accompany them remotely and help them through the process. This is what the co-founders of Kidopi, a startup based in Ribeirão Preto (São Paulo state, Brazil), thought when they developed a digital companion, available on WhatsApp, that provides information and guidance while acting as a guardian. The solution was created with the support of FAPESP’s Innovative Research in Small Businesses Program (PIPE).
The startup’s co-founder and CEO, Mario Sérgio Adolfi Junior, says that the idea was to provide an accessible and easy-to-use tool for patients. “Ever since I started university, I wanted to use my knowledge to make an impact on health on a large scale,” he recalls. “We chose WhatsApp because it’s a widely used platform, it’s familiar to patients, and it doesn’t require any downloads or complicated interfaces.”
The researcher explains that the company develops medical IT solutions. “We work in the health informatics segment, especially in the patient journey,” he says. “Our focus is on ensuring patient care because many problems can be solved outside the hospital if they have the right support.”
Different journeys
According to Adolfi Junior, the tool is very versatile and allows the creation of specific journeys according to the needs of each user. “I realized that the big challenge is that patients don’t have enough follow-up after leaving the hospital. They often don’t know if they have any serious symptoms and the result is repeated visits to the health unit,” he states.
For example, after surgery, Kidopi’s system can monitor the patient to find out how they are recovering and remind them to take their medication. The follow-up includes daily questions to find out if the recovery is going well. “From this, it’s possible to know if the progress has been as it should be. If anything goes wrong, the patient is told to go to the hospital. It’s as if we’re holding their hand and guiding them all the way.”
All of this conversation takes place fluidly over WhatsApp, as the system uses natural language processing – allowing the user to interact as if they were in contact with a healthcare professional. “Because the user is talking on WhatsApp, an app they’re used to, adherence is high. They talk the way they’re used to, and the system understands and guides them through the process.”
The results show that the tool is effective. Adolfi Junior says that of the users who were told to stay home, 100% had no problems. “Of those who went to the hospital, 75% should have gone there. These were cases where there was a serious point and intervention was needed,” he says. “In a project we did in partnership with the A.C.Camargo hospital and Johnson & Johnson, because the patients went to the health unit early, there was a 67% reduction in surgical complications.”
Standby team
If the user is told to go to the health unit, the entire history of their conversation with the system is sent to the doctor who will see them. “It’s all interconnected. Everything goes to a hospital switchboard, which gets an alert that the patient is on their way, as well as information about what happened. If necessary, a health professional can contact them for more information.”
According to the researcher, this is a way to ensure the patient’s quality of life while reducing the risk of death and hospitalization. “It’s a win-win process because the hospital offers a form of care that differentiates it from other hospitals. It can then attract partners precisely because it offers that differential.”
He points out that the tool delivers information to patients exactly when they need it. And one of its highlights is its ability to humanize care. “We have feedback from a project involving the Hospital de Amor in Barretos [state of São Paulo, about 120 km from Ribeirão Preto] and Roche, which shows that users feel comfortable with the solution. They often say: ‘Can I add a friend who has just been diagnosed to the program? I have, and it makes me feel very safe. I feel like someone is looking out for me.’ It’s very gratifying.”
Other uses
The versatility of the solution allows it to be used in other situations in addition to monitoring patients after surgery. Kidopi has programs for diabetes, cancer, osteoporosis and other chronic conditions. It also monitors the elderly and those seeking well-being, such as weight loss. “We monitor the elderly to ensure a better quality of life and prevent complications. It’s a comprehensive approach that takes into account the mental and emotional health of the caregivers,” he explains.
The executive highlights the possibility of hyper-personalizing the solution. It can therefore be adapted to different profiles and needs. “Patients have specific needs. For a woman going through menopause, for example, the approach needs to take into account that time of life. The caregiver of a frail elderly person, on the other hand, needs information about home safety, how to identify risks in the environment and, of course, self-care to deal with the stress of the job.”
Because the platform uses artificial intelligence to customize each patient’s journey, personalization is based on the patient’s unique characteristics and the moment they are in. “Our solution isn’t fixed, in other words, it isn’t a system that works in the same way for everyone,” he explains. “It’s important that each individual gets the care they really need at each stage of their treatment or condition.”
On the road to internationalization
Today, Kidopi’s solution is already in the hands of thousands of patients. “FAPESP was essential for us to be able to turn an academic project into a company,” says Adolfi Junior.
The company is now preparing to expand internationally, with a new PIPE project to develop Spanish and English versions of the solution. “We’re happy to have opened our company in the state of São Paulo and to have the support to make our technology globally competitive.”
The startup was one of those selected to participate in a business mission during FAPESP Week Spain, which took place from November 27 to 28 at the Faculty of Medicine of the Complutense University of Madrid (UCM) in the Spanish capital.
The researcher believes that digital medicine has great potential, especially for patients who require constant care, such as the elderly. “The world is aging rapidly, and solutions like ours will be essential to ensure that the elderly can receive continuous, high-quality care without having to be constantly hospitalized.”
While the digital solution doesn’t replace the doctor or specialized care, it can complement and support them by providing a safety net for the patient. In this way, technology can help improve care, prevent complications, and provide continuous follow-up wherever the individual is.
The service is always free to the patient – the cost is borne by the healthcare provider, such as a hospital, pharmaceutical company or health plan. This improves adherence and democratizes access to care.
